Anorectal examination
A spinal cord injury can be assessed through an anorectal examination. This examination can be done in two ways – a peri-anal sensory examination and/or a digital rectal examination.
Peri-anal sensory examination
The peri-anal examination is required to complete the International Standards for Neurological Classification of Spinal Cord Injury assessment. This assessment involves sensory grading of the S4-5 dermatome for light touch and pin prick.
For more information on how to conduct this assessment:
American Spinal Injury Association, The premier North American organisation in the field of Spinal Cord Injury Care, Education, and Research.
Digital rectal examination
A digital rectal examination is to assess deep anal pressure, voluntary anal contraction and anal reflexes.
Deep anal pressure and voluntary anal contraction
The assessment of deep anal pressure and voluntary anal contraction is required to complete the International Standards for Neurological Classification of Spinal Cord Injury assessment.
For more information on how to conduct this assessment:
American Spinal Injury Association, The premier North American organisation in the field of Spinal Cord Injury Care, Education, and Research.
International standards for neurological classification of spinal cord injury (ISNCSCI) worksheet – This is commonly referred to as the ASIA form
Anal reflexes
This examination is not required for The International Standards for Neurological Classification of Spinal Cord Injury assessment; however, it enables the differentiation between upper motor neurone and lower motor neurone spinal cord injuries, as well as spinal shock. On this bases, the anal reflexes examination is important for determining an appropriate bowel management plan.
Check person’s identification. Explain to the person that a gloved and lubricated finger will be inserted 2-3 cm into the rectum.
Spinal shock
Spinal shock is a temporary loss of all, or most, reflex activity, as a result of a high-level spinal cord injury usually (T6 and above).
Spinal shock typically lasts for 48 to 72 hours and sometimes for weeks or months.
A spinal shock can cause an areflexic rectum and anus, and/or absent colon peristalsis, resulting in paralysis of the intestines that can lead to a bowel obstruction (known as paralytic ileus).
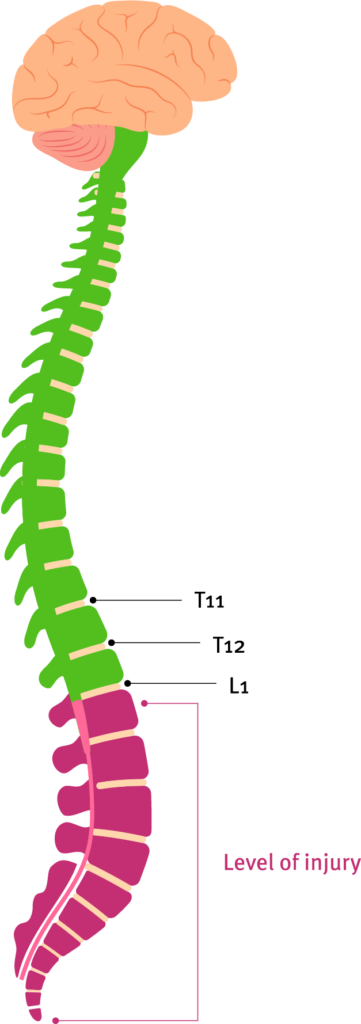
Upper motor neurone injury
An upper motor neurone (UMN) type bowel most commonly occurs in people with spinal cord injuries above T12/L1. This type of bowel is influenced by the intact action of the defecation reflex centre, which causes an involuntary spasm-like contraction of the muscles in the rectum and anus.
However, given that spinal cord injury can disrupt the message pathways up and down the spinal cord, people with UMN spinal injuries are unable to control the relaxing of these muscles to allow or prevent defecation. They also may have difficulty determining whether their bowel is full or has already evacuated, or whether wind and/or solid matter has been passed.
Left untreated, people with UMN-type bowels will likely experience chronic constipation and recurring, unplanned bowel movements. This can impact other key facets of health, work and social life, as well as personal relationships.
Injury occurs in the cord above the conus (T12-L1 level). There is a general loss of voluntary control below the level of injury (pending neurological impairment).
Stimulus eg. Filling bladder, stool in lower rectum, touched on leg
Muscle
Reflex stimulated at cord
Spasm triggered at muscle and muscles contract e.g. detrusor, bladder or bowel sphincters spasm closed, skeletal muscles
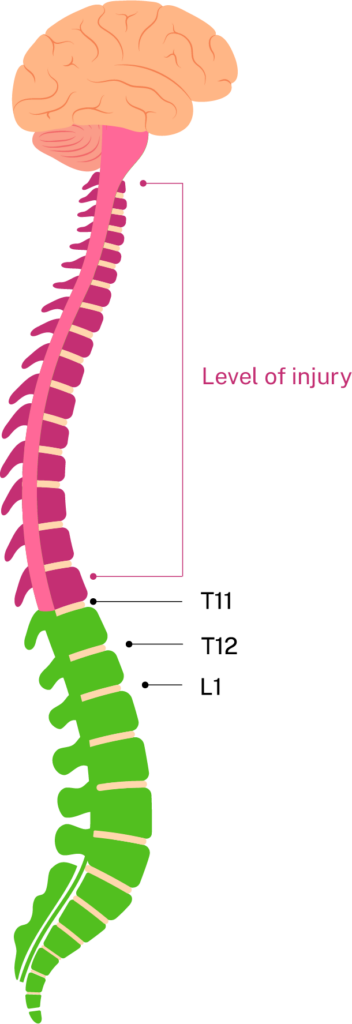
Lower motor neurone injury
Lower motor neurone (LMN) or cauda equina syndrome (CES) type bowels most commonly occur in people with spinal cord injuries at or below T12/L1.
In these bowel types, messages to the defecation reflex centre (located below T12/L1) are disrupted, leaving it unable to exert any influence over the anal and rectal muscles, resulting in a flaccid bowel. This means people with LMN spinal injuries generally have:
- poor or no anal tone
- loss of voluntary control
- poor or no sensation of the lower bowel, to know when it is full or when an evacuation has occurred
- decreased peristalsis.
Left untreated, people with LMN bowels can experience chronic constipation and unplanned bowel movements.
Uncontrolled bowel motions (faecal incontinence) increase the risk of skin breakdown, as well as problems with incontinence-associated dermatitis (IAD). Excessive stool contact with the skin causes overhydration and an increased pH of the skin. This can impact other key facets of health, work and social life, as well as personal relationships.
Injury occurs below cord at conus (T12-L1 level). There is general loss of voluntary control below the level of injury (pending neurological impairment).
Stimulus eg. Filling bladder, stool in lower rectum, touched on leg
Muscle
No reflex activity
Flaccid paralysis eg. low tone of detrusor, bladder or bowel sphincters, skeletal muscles