Approach to supporting sexuality
Sexuality is defined by the World Health Organization as:
“…a central aspect of being human throughout life encompasses sex, gender identities and roles, sexual orientation, eroticism, pleasure, intimacy and reproduction. Sexuality is experienced and expressed in thoughts, fantasies, desires, beliefs, attitudes, values, behaviours, practices, roles and relationships. While sexuality can include all of these dimensions, not all of them are always experienced or expressed. Sexuality is influenced by the interaction of biological, psychological, social, economic, political, cultural, legal, historical, religious and spiritual factors.”
Sexual health is defined by the World Health Organization as:
“a state of physical, emotional, mental and social well-being in relation to sexuality; it is not merely the absence of disease, dysfunction or infirmity. Sexual health requires a positive and respectful approach to sexuality and sexual relationships, as well as the possibility of having pleasurable and safe sexual experiences, free of coercion, discrimination and violence. For sexual health to be attained and maintained, the sexual rights of all persons must be respected, protected and fulfilled.”
Frameworks for supporting sexuality
The Sexual Rehabilitation Framework (SRF) encourages all disciplines to be involved in SCI rehabilitation in the same manner as they would other activities of daily living. It addresses the major biopsychosocial areas of sexuality to create a plan of action for the person with SCI.
The original PLISSIT and Extended-PLISSIT models are useful frameworks to guide multidisciplinary teams in addressing the sexual wellbeing of people with SCI. The models empower healthcare professionals to integrate sexuality into routine care, recognizing that it is a fundamental part of life.
In the original PLISSIT model, the name PLISSIT is an acronym representing four levels of intervention:
- P – Permission: Create a safe, non-judgmental environment that encourages patients to discuss sexuality.
- LI – Limited Information: Provide specific, relevant information related to the client’s concerns.
- SS – Specific Suggestions: Offer tailored strategies based on the individual’s needs. This requires a more in-depth understanding of the person’s situation and the impact of spinal cord injury on sexuality.
- IT – Intensive Therapy: Offer therapy where this is within professional scope or refer to a specialist if the issue is beyond scope.
The Extended PLISSIT (Ex-PLISSIT) model modifies and improves upon the original by:
- Emphasizing “Permission-giving” at all stages, not just the first.
- Incorporating reflection and feedback loops, encouraging practitioners to be more self-aware and person-centred.
- Recognizing that sexuality is a lifelong, dynamic part of human experience, even after events like spinal cord injury or chronic illness.
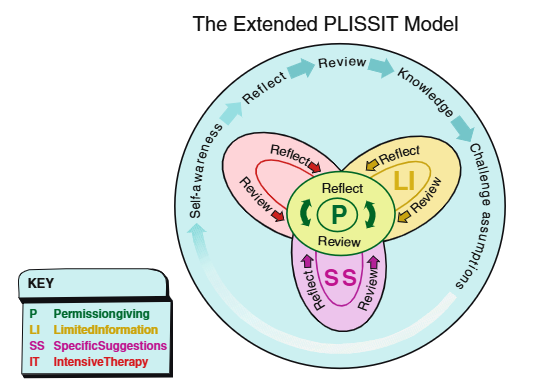
The Ex-PLISSIT model
Source: Taylor and Davis (2007)
Core principles for supporting sexuality
Sexual and reproductive health is a vital part of overall well-being and should be included in routine healthcare and rehabilitation planning. Health professionals can support people with spinal cord injury (SCI) and their partner/s, where relevant, by following these key principles:
- Recognise individuality: Every person is unique, with their own identity, relationships, life experiences, needs and preferences.
- Use inclusive and respectful language: Communicate in a way that is open, respectful, and accessible to everyone, regardless of gender, sexuality or relationship status.
- Offer holistic and team-based support: Ensure that sexual health education and support are available from the broader multidisciplinary team and consider physical, psychological, and social factors, within a biopsychosocial model.
- Include sexual health in routine care: Discussions should address areas such as sexual desire, function, fertility, contraception, body image and relationships.
- Promote a positive culture: Foster a work environment that values sexual well-being and encourages staff to seek training in sexual health and sexuality in the context of SCI and disability.
Assessing sexual health and function
Comprehensive SCI care includes access to a health professional whose scope of practice includes the assessment of sexual health and function. This assessment may include:
- Taking a thorough history: Include questions about sexual function, concerns, goals, and any changes since the injury.
- Conducting a physical exam if needed: This helps assess physical changes and establish a baseline for future care.
- Encouraging routine screening: Include health checks such as cervical screening tests, breast exams, and testicular or prostate exams.
Promoting safe and healthy sexual activity
- Provide clear education: Talk about consent, contraception options, and the use of condoms to reduce the risk of sexually transmitted infections (STIs) and unplanned pregnancies.
- Support informed decision-making: Help people with SCI understand their sexual health options and empower them to explore what works best for their individual situation and relationships.
Sex after spinal cord injury: the sexual health framework
Spinal Cord Injury Research Evidence (SCIRE)
Sex after spinal cord injury: using the PLISSIT model to address sexual health
Spinal Cord Injury Research Evidence (SCIRE)
The extended PLISSIT (Ex-PLISSIT) model
Taylor and Davis, Sexuality and Disability Journal
Undressing sex: how to have sexuality conversations in practice
University College London with Lynch & Allatt
Let’s talk about sex – sharing sexuality education resources for occupational therapists
Let’s Talk About Sex
Sexual and reproductive health following spinal cord injury
SCIRE Professional: Spinal Cord Injury Research Evidence
Sexuality following spinal cord injury
New South Wales Government Agency for Clinical Innovation (NSW ACI)
Fertility following spinal cord injury
New South Wales Government Agency for Clinical Innovation (NSW ACI)
SCI sexual health
Spinal Cord Injury British Colombia (SCI BC)
Sexuality after SCI
Mount Sinai Hospital
Social work and psychosexual therapy resources
Care Rehab
Understanding sexual dysfunction in spinal cord injury
Mens Health Downunder
The use of vibrators and clitoral stimulators
Mens Health Downunder
Sexuality and sexual functioning after SCI
Model Systems Knowledge Translation Centre (MSKTC)
Sexual aids
National Equipment Database (AskNED)
pleasureABLE Sexual device manual for persons with disabilities
MacHattie et al, Disabilities Health Research Network
The MA+ guide: a guide to more accessible sexuality-related assistive technology
Narelle Higson, the Multiple Sclerosis Society of Western Australia
Sexual positions for women with paralysis: creativity, adaptability and sense of humour
Dr Mitchell Tepper, Regain That Feeling
Gottman card decks app: a relationship app
The Gottman Institute
Sexual self-discovery and body mapping tool
University Health Network – Toronto Rehab
Assistive tech unveiled: solutions for enhanced bedroom pleasure
Spinal Cord Injuries Australia (SCIA)
Sexuality and fertility following spinal cord injury
Spinal Cord Injuries Australia (SCIA)
Sex and fertility information
Facing Disability for families facing spinal cord injury
Sexuality and reproductive health in adults with spinal cord injury: what you should know
Consortium for Spinal Cord Medicine
Occupational performance inventory of sexuality and intimacy (OPISI)
University of Indianapolis
5 disability-inclusive sex positions to spice up the bedroom
The Mighty
Agency for Clinical Innovation. (2017). Fertility following spinal cord injury. NSW Government. https://aci.health.nsw.gov.au/__data/assets/pdf_file/0006/600855/ACI-Fertility-following-spinal-injury.pdf
Agency for Clinical Innovation. (2014). Sexuality following spinal cord injury: A guideline for health professionals. NSW Government. https://aci.health.nsw.gov.au/__data/assets/pdf_file/0004/349051/ACI-Spinal-sexuality-guideline.pdf
Alexander, M., Courtois, F., Elliott, S., & Tepper, M. (2017). Improving Sexual Satisfaction in Persons with Spinal Cord Injuries: Collective Wisdom. Topics in spinal cord injury rehabilitation, 23(1), 57-70. https://doi.org/10.1310/sci2301-57
Australian Government Department of Health and Aged Care. (n.d.). About sexual health. Retrieved May 24, 2025, from https://www.health.gov.au/topics/sexual-health/about
Bryant, C., Aplin, T., & Setchell, J. (2022). Sexuality Support After Spinal Cord Injury: What is Provided in Australian Practice Settings? Sexuality and Disability, 40(3), 409-423. https://doi.org/10.1007/s11195-022-09756-w
Bryant, C., Gustafsson, L., Aplin, T., & Setchell, J. (2021). Supporting sexuality after spinal cord injury: A scoping review of non-medical approaches. Disabil Rehabil, 44(19):5669-5682. https://doi.org/10.1080/09638288.2021.1937339
Earle, S., O’Dell, L., Davies, A., & Williams, R. (2020). Views and experiences of sex, sexuality and relationships following spinal cord injury: A systematic review and narrative synthesis of the qualitative literature. Sexuality and Disability, 38(4), 567–595. https://doi.org/10.1007/s11195-020-09653-0
Elliott, S., Hocaloski, S., & Carlson, M. (2017). A Multidisciplinary Approach to Sexual and Fertility Rehabilitation: The Sexual Rehabilitation Framework. Topics in spinal cord injury rehabilitation, 23(1), 49-56. https://doi.org/10.1310/sci2301-49
Elliott, S., & Querée, M. (2018). Sexual and reproductive health following spinal cord injury. In J. J. Eng, R. W. Teasell, W. C. Miller, D. L. Wolfe, A. F. Townson, J. T. C. Hsieh, S. J. Connolly, V. K. Noonan, E. Loh, S. Sproule, A. McIntyre, & M. Querée (Eds.), Spinal cord injury rehabilitation evidence (Version 6.0, pp. 1–133). SCIRE Project. https://scireproject.com/wp-content/uploads/2022/04/SCIRE-Sexual-Health-Version-6-chapter_Nov.23.18-v.FINAL-2.pdf
Lynch, C., & Fortune, T. (2019). Applying an Occupational Lens to Thinking About and Addressing Sexuality. Sexuality and Disability, 37(2), 145-159. https://doi.org/10.1007/s11195-019-09566-7
Henke, A. M., Billington, Z. J., & Gater, D. R., Jr (2022). Autonomic Dysfunction and Management after Spinal Cord Injury: A Narrative Review. Journal of personalized medicine, 12(7), 1110. https://doi.org/10.3390/jpm12071110
Paralyzed Veterans of America. (2012). Sexuality and reproductive health in adults with spinal cord injury: A clinical practice guideline for health care professionals. https://pva.org/wp-content/uploads/2021/09/sexuality-consumer-cpg-2012.pdf
Parker, M. G., & Yau, M. K. (2012). Sexuality, Identity and Women with Spinal Cord Injury. Sexuality and Disability, 30(1), 15-27. https://doi.org/10.1007/s11195-011-9222-8
Taylor, B., Davis, S. The Extended PLISSIT Model for Addressing the Sexual Wellbeing of Individuals with an Acquired Disability or Chronic Illness. Sex Disabil 25, 135–139 (2007). https://doi.org/10.1007/s11195-007-9044-x
World Health Organization. (n.d.). Sexual health. Retrieved May 24, 2025, from https://www.who.int/health-topics/sexual-health#tab=tab_2