Respiratory changes
There are numerous aspects to respiratory function change following an acute spinal cord injury (SCI).
These may include:
- respiratory neuromuscular weakness involving the intercostals, abdominals and possibly even the diaphragm
- reduced diaphragm efficiency due to altered chest wall and abdominal muscle tone and compliance
- restricted inspiratory capacity and decreased forced expiratory volumes and flow rates
- impaired sigh, cough and other forced expiratory actions
- atelectasis and sputum retention
- hypoventilation, which may progress to hypoxaemia and hypercapnia
- increased work of breathing due to altered breathing mechanics—especially in sitting
- increased risk of respiratory fatigue and failure, as well as sleep-disordered breathing.
In summary, these changes collectively lead to reduced ventilation and secretion clearance, while also increasing the work of breathing.
Reduced ventilation and secretion clearance
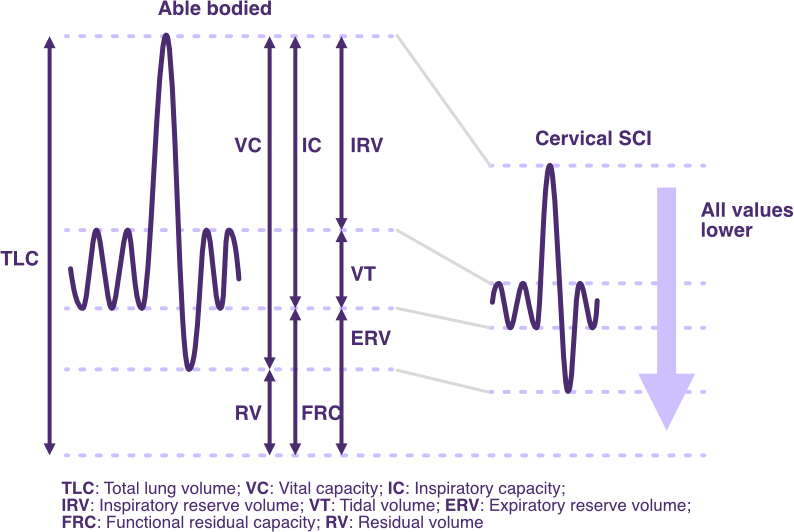
Changes in spirometry lung volumes and capacities following SCI
Adapted from SCIRE Professional
Following a SCI at or above the neurological level of T12, some degree of respiratory muscle weakness or paralysis occurs involving the intercostal and abdominal muscles.
At very high neurological levels of injury (NLI)—C5 or above—weakness or paralysis of the diaphragm may result, involving either one or both hemi-diaphragms. Other accessory respiratory muscles may also be impaired.
The degree of respiratory muscle impairment will correlate with a reduction in tidal and inspiratory reserve volumes, as well as expiratory volumes and flow rates.
Reduced inspiratory volumes impact gas exchange and surfactant production, promoting atelectasis and diminishing minute ventilation.
Reduced expiratory volumes impact the capacity to sigh and cough effectively, promoting rising CO2 and retained secretions.
Over time, significant and sustained hypoventilation can cause hypoxaemia and hypercapnia, promote ventilation–perfusion mismatch, and increase the risk of respiratory complications.
Increased work of breathing
The work of breathing typically increases due to:
- paradoxical breathing
- increased airway and/or inspiratory resistance
- any compensatory responses to declining ventilation, such as an increased respiratory drive and accessory muscle recruitment
- other activities related to personal and medical care.
Paradoxical breathing
Any altered breathing pattern, especially paradoxical breathing, significantly increases the work of breathing.
In the acute stage following SCI, spinal shock is present.
In addition to amplifying any weakness or paralysis of the intercostal and abdominal muscles, muscle function is further impaired by the presence of flaccid tone and increased compliance.
A paradoxical breathing pattern typically develops during inspiration.
The impact of these changes—strength, tone, compliance—on respiratory breathing mechanics are described below.
Intercostal muscle paralysis with flaccidity and increased compliance:
- causes increased chest wall compliance and instability
- leads to anterior chest wall depression and intercostal space recession from the increasing negative intrathoracic pressure during inspiration, as the diaphragm contracts and descends
- prevents effective chest wall expansion from full diaphragm contraction during the last phase of inspiration, limiting inspiratory reserve volume.
Abdominal muscle paralysis with flaccidity and increased compliance:
- leads to excessive abdominal wall compliance
- allows abdominal contents to fall away from the diaphragm—especially when sitting—affecting diaphragm shaping and a pronounced abdominal rise during inspiration
- results in the diaphragm contracting from a flattened rather than domed shape, compromising its optimal length-tension relationship and reducing its excursion range, generating a lower tidal volume.
Increased diaphragm inefficiency and ventilation load:
- occurs as the NLI becomes higher because
- diaphragm function becomes increasingly impaired from changes to intercostal and abdominal muscle function
- inspiration is increasingly dependent on diaphragm function alone
- significantly increases the work of breathing
- results in hypoventilation, increasing the risk of respiratory fatigue and eventual respiratory failure.
Paradoxical breathing is a “see-saw” movement pattern between the chest wall and abdomen during inspiration. It is characterised by:
- depression of the anterior chest wall
- recession between the intercostal spaces
- pronounced abdominal rise.
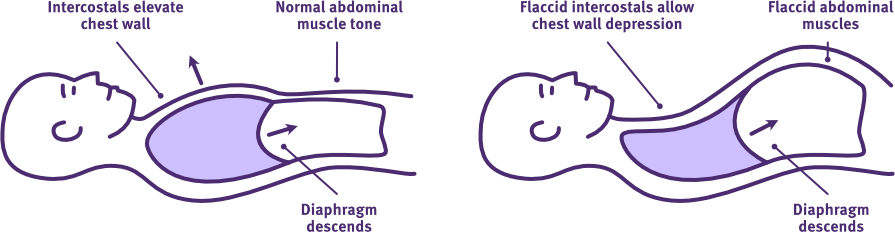
The normal versus paradoxical breathing pattern following acute high-level SCI
Adapted from Thoracic Key
The following video illustrates paradoxical breathing following an acute high-level SCI.
Airway and inspiratory resistance
Any increased airway and/or inspiratory resistance significantly increases the work of breathing.
The respiratory effort must generate a greater pressure differential to overcome this to maintain adequate inspiratory volumes and flow rates, which determine minute ventilation.
Increased airway and/or inspiratory resistance may arise from:
- autonomic nervous system (ANS) disruption, such as bronchospasm and increase sputum production
- concomitant injuries, including pneumathoraces and rib fractures
- respiratory complications, including atelectasis and pulmonary oedema
- abdominal complications, including paralytic ileus/constipation
- comorbidities with ageing, including rigid chest wall/fibrosed lung.
Compensatory responses
Any increased respiratory drive and accessory muscle recruitment further increases the work of breathing.
To compensate for diminished minute ventilation and the onset of hypercapnia, the body typically increases respiratory drive.
This often results in an elevated respiratory rate and greater recruitment of accessory muscles during quiet and deeper breathing.
Other
In addition to the effect of respiratory function changes following SCI, other activities associated with personal and acute medical care, may add to the work of breathing.
This is particularly applicable to the hospital environment, where routine activities can be continually interruptive and significantly compound both energy expenditure and sleep-deprivation. In turn, this can increase both the work of breathing and limit restorative rest.
Activities to be mindful of include:
- assessment demands
- patient speech e.g. to answer subjective questions, communicate with family and friends
- repeated assessments e.g. across the multi-disciplinary team, for ward admissions, during shift changes
- high-demand respiratory assessments e.g. spirometry, cough effectiveness
- positioning and positioning changes e.g. radiology
- management interventions
- general cares e.g. hygiene, feeding, hoisting and general patient transport
- positioning and positioning changes e.g. pressure rolls, postural drainage, inappropriate sitting, theatre
- chest physiotherapy treatment sessions e.g. long treatments, ineffective attempts at coughing
- medical changes to respiratory airway e.g. intubation and extubation.
While many of these activities are unavoidable, the overall energy expenditure and quality of rest should be carefully monitored to manage the risk of respiratory fatigue.
The impact of respiratory changes
A substantial increase in the work of breathing is the precursor to the onset of respiratory fatigue.
Similarly, significant and sustained hypoventilation can progress to hypoxaemia and hypercapnia, and is the precursor to the onset of respiratory failure.
Without early management planning for timely and appropriate intervention, the onset of respiratory fatigue will quickly progress to respiratory failure (typically occurs between 1-5 days following high-level cervical SCI).
For more information on management interventions, refer to Acute management, Ventilation support, Lung volume augmentation and Secretion management.
The impact of time
Beyond the acute management phase following a SCI, respiratory function will improve with any respiratory muscle recovery and strengthening which occurs due to neural plasticity and rehabilitation. However, it also improves as spinal shock resolves in the weeks and months post-injury. This may be due to:
- the NLI improving and resulting in improved respiratory muscle strength generally
- any intercostal and abdominal muscle flaccidity transitioning to spasticity, so that it
- reduces excessive chest wall and abdominal compliance
- helps correct a paradoxical breathing pattern
- decreases the work of breathing
- any ANS disruption (parasympathetic nervous system (vasovagal) dominance) being partially rebalanced, correcting negative respiratory and cardiovascular effects.
When changes to respiratory dysfunction have stabilised, weaning from ventilation supports and progression to sitting may be introduced.
However, any residual respiratory dysfunction will continue to require ongoing management to optimise ventilation and secretion clearance, while reducing the work of breathing.
Over time, other management issues may also emerge related to chronic respiratory dysfunction and ageing.
Respiratory impairment in SCI (2025)
PM&R KnowledgeNow
Respiratory management (rehab phase) (2022)
SCIRE Professional
eLearn SCI— physiotherapists—respiratory: assessing and treating module
eLearn SCI.org
Berlowitz, D. J., Wadsworth, B., & Ross, J. (2016). Respiratory problems and management in people with spinal cord injury. Breathe (Sheff), 12(4), 328–340. https://doi.org/10.1183/20734735.012616
Brown, R., DiMarco, A. F., Hoit, J. D., & Garshick, E. (2006). Respiratory dysfunction and management in spinal cord injury. Respiratory Care, 51(8), 853-870. https://doi.org/10.4187/respircare.05185
Denton, M., & McKinlay, J. (2009). Cervical cord injury and critical care. Continuing Education in Anaesthesia, Critical Care & Pain, 9(3), 82–86. https://doi.org/10.1093/bjaceaccp/mkp013
Fogarty, M. J., & Sieck, G. C. (2020). Spinal cord injury and diaphragm neuromotor control. Expert Review of Respiratory Medicine, 14(5), 453–464. https://doi.org/10.1080/17476348.2020.1732822
Galeiras Vázquez, R., Rascado Sedes, P., Mourelo Fariña, M., Montoto Marqués, A., & Ferreiro Velasco, M. E. (2013). Respiratory management in the patient with spinal cord injury. BioMed Research International, 2013, Article 168757. https://doi.org/10.1155/2013/168757
Harvey, L. A. (2008). Management of spinal cord injuries: A guide for physiotherapists. Churchill Livingstone Elsevier.
Hendershot, K. A., & O’Phelan, K. H. (2023). Respiratory complications and weaning considerations for patients with spinal cord injuries: A narrative review. Journal of Personalized Medicine, 13(1), 97. https://doi.org/10.3390/jpm13010097
Krassioukov A. Autonomic function following cervical spinal cord injury. Respir Physiol Neurobiol. Nov 2009;169(2):157-64. https://doi:10.1016/j.resp.2009.08.003
Randelman, M., Zholudeva, L. V., Vinit, S., & Lane, M. A. (2021). Respiratory training and plasticity after cervical spinal cord injury. Frontiers in Cellular Neuroscience, 15, Article 700821. https://doi.org/10.3389/fncel.2021.700821
Yartsev, A. (2015, June 30). Physiological consequences of spinal cord transection. Deranged Physiology. https://derangedphysiology.com/main/required-reading/trauma-intensive-care/Chapter-210/physiological-consequences-spinal-cord-transection
Zimmer, M. B., Nantwi, K., & Goshgarian, H. G. (2007). Effect of spinal cord injury on the respiratory system: Basic research and current clinical treatment options. The Journal of Spinal Cord Medicine, 30(4), 319–330. https://doi.org/10.1080/10790268.2007.11753947