Respiratory predictive factors
Following a spinal cord injury (SCI), multiple predictive factors determine the extent of respiratory dysfunction. Increasing prevalence or severity of these factors correlates with more significant changes in respiratory function and a higher risk of developing complications, particularly in the early post-injury period. Some factors are specific to the acute phase, whereas others persist life-long.
A comprehensive respiratory assessment assists in identifying these factors and supports early management planning for timely and appropriate intervention. Typically, it is imperative to improve ventilation and secretion clearance, while reducing the work of breathing. This is both relevant during the acute management of SCI, and when a person with chronic SCI becomes acutely unwell.
Key predictive factors are the neurological level of injury (NLI), along with the degree of motor impairment and autonomic nervous system (ANS) disruption. Other predictive factors are the presence of spinal shock, concomitant injuries, medical issues and comorbidities associated with age.
The International Standards for Neurological Classification of Spinal Cord Injury (ISNCSCI) can be used to as a starting point to determine both the NLI and degree of motor impairment. However, it does not:
- include specific motor tests to grade the strength of the trunk, neck or head muscles involved in respiration (when assessing these body areas, it infers that impaired sensation of a dermatome indicates impaired motor function of the associated myotome)
- determine the degree of ANS disruption, so this must be determined symptomatically.
ISNCSCI explained
The Neurological Level of Injury (NLI) is defined as the lowest segment of the spinal cord with intact sensory and motor function on both sides of the body, provided function is normal in all segments above.
- Motor function is considered intact if the key muscles at that level have a strength of at least grade 3 (antigravity), with grade 5 (normal) strength in all levels above.
- Sensory function must be normal (score of 2) for both light touch and pin prick on both sides at that level and above.
An ASIA Impairment Scale (AIS) is then determined based on sensory and motor scores and the presence or absence of sacral sparing (anal sensation or voluntary anal contraction).
- It classifies the injury from AIS A (complete) to AIS E (normal), reflecting the degree of preserved neurological function below the injury level.
The ISNCSCI classification (including the AIS grade) does not assess autonomic nervous system (ANS) function.
While an AIS A injury often suggests a complete sympathetic disruption at that level, this is not always the case. Therefore, ISNCSCI should be supplemented by separate evaluations of autonomic function to assess any ANS disruption.
Neurological level of injury
The NLI represents the lowest neurological level of intact spinal nerve root innervation.
A NLI above T12 predicts some respiratory muscle impairment, increasing as the NLI becomes higher.
For example, a NLI of C5 will likely result in greater respiratory dysfunction than a NLI of T5.
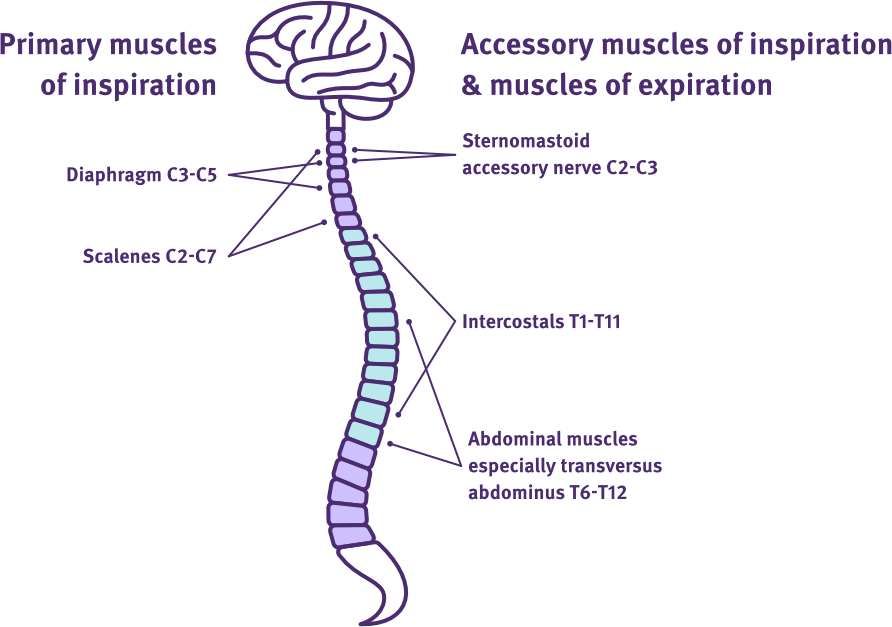
Respiratory muscles and spinal nerve root innervations
Adapted from SCIRE Professional
Degree of motor impairment
In addition to determining the NLI, the ISNCSCI assigns an impairment grade (AIS A–E) to describe the severity of motor and sensory loss.
A higher NLI, together with a greater degree of motor impairment, predicts more significant respiratory muscle weakness or paralysis.
For example, a C5 AIS A injury will likely result in greater respiratory dysfunction than a C5 AIS D injury.
NLI above T12 → increasing paralysis of lower intercostal and lower abdominal muscles.
NLI above T6 → increasing paralysis of intercostal muscles, with full paralysis of all abdominal muscles.
NLI at C5 or above → increasing paralysis of the diaphragm and some accessory muscles, with full paralysis of all intercostal and abdominal muscles.
NLI at C2 or above → increasing paralysis of respiratory accessory muscles, with full paralysis of all intercostal, abdominal and diaphragm muscles i.e. nil spontaneous breathing.
Specifically, the extent of abdominal, intercostal and diaphragm muscle weakness or paralysis, will determine:
- the reduction of tidal and inspiratory reserve volumes, as well as the overall impairment to diaphragm functioning and efficiency
- the reduction of forced expiratory volumes and flow rates, affecting the regulation of carbon dioxide (CO₂) levels and the ability to clear secretions.
Overall, the degree of these changes exponentially diminish minute ventilation and increase the work of breathing, along with the risk of respiratory complications.
Degree of autonomic nervous system disruption
The autonomic nervous system (ANS) controls many of the body’s involuntary functions.
These functions occur automatically, without conscious effort.
A SCI can disrupt the connection between the brain and autonomic pathways, leading to an imbalance in the ANS.
A NLI at or above T6 can disrupt sympathetic nervous system inputs which include regulation of various respiratory and cardiovascular functions—instead parasympathetic nervous system activity dominates.
For more information on ANS disruption, refer to Autonomic nervous system.
If the NLI is at or above T6, the presence of autonomic nervous system (ANS) disruption predicts additional respiratory and cardiovascular effects. For example, these may be:
- increased sputum production
- bronchospasm
- nasal congestion
- arrhythmias, especially bradycardia
- reduced cardiac output
- increased risk of pulmonary embolism and pulmonary oedema.
Overall, the presence of ANS disruption in addition to respiratory muscle impairment, may further diminish minute ventilation and increase the work of breathing, along with the risk of respiratory complications.
Spinal shock
Spinal shock is a temporary condition that occurs immediately after a spinal cord injury, typically lasting 4 to 6 weeks.
It results in:
- a complete loss of sensation as well as muscle activity, tone and reflexes below the level of injury
- impaired autonomic nervous system function of all associated body organs—impacting sputum production, bronchial tone, heart rate regulation, vascular tone, blood pressure, bladder, and bowel activity.
For more information on spinal shock, refer to Neurogenic and spinal shock.
Spinal shock occurs in the acute phase following SCI and when present, predicts more significant respiratory dysfunction.
It amplifies the impact of the NLI on respiratory muscle function, including the degree of motor impairment and ANS disruption.
In addition to this, any respiratory muscle weakness or paralysis presents with flaccid muscle tone and this further alters breathing mechanics.
For example, flaccidity of the weakened or paralysed intercostal and abdominal muscles increases chest and abdominal wall compliance. This further reduces the functioning and efficiency of the diaphragm during inspiration, especially in sitting.
Typically, a paradoxical breathing pattern develops during inspiration, evidenced by a collapse of the chest wall, with a simultaneous heightened rise of the abdomen.
Overall, the presence of spinal shock with respiratory dysfunction will further diminish minute ventilation and increase the work of breathing, along with the risk of respiratory complications. This is until the overlay of spinal shock resolves in the following weeks and months post-injury.
Concomitant injuries
Other factors which may further compound respiratory dysfunction in the acute phase are:
- high-velocity or high-force trauma resulting in chest wall or abdominal injury
- risk of aspiration, including immersion injuries or excessive saliva production with some degree of dysphagia
- traumatic brain injury
- pain
- altered level of consciousness
- altered psychological state
- post-surgical recovery (e.g. spinal discectomies, fusions, intra-abdominal repairs)
- prolonged invasive ventilation or recent extubation
- use of medications, particularly opioids
- faecal impaction due to paralytic ileus or severe constipation, limiting diaphragm excursion and increasing the work of breathing
- complications from other body systems, such as fluid or electrolyte imbalances, or hypoalbuminemia.
Medical issues
Other factors which may further compound respiratory dysfunction in the acute phase are:
- post-surgical recovery (e.g. spinal discectomies, fusions, intra-abdominal repairs)
- prolonged invasive ventilation or recent extubation (e.g. ventilator associated pneumonia (VAP) and ventilator-induced diaphragmatic dysfunction (VIDD))
- use of medications, particularly opioids
- faecal impaction due to paralytic ileus or severe constipation, limiting diaphragm excursion and increasing the work of breathing
- complications from other body systems, such as fluid or electrolyte imbalances, or hypoalbuminemia.
Comorbidities and ageing
Other factors which may further compound respiratory dysfunction in the acute phase are:
- age > 50 years
- body mass index (BMI) > 25
- history of smoking
- chronic lung diseases
- pre-existing cardiovascular, neurological or musculoskeletal conditions
- mental health conditions or intellectual disability.
Predictors for respiratory function in SCI
SCIRE Professional
Respiratory management (rehab phase)
SCIRE Professional
Aarabi, B., Harrop, J. S., Tator, C. H., Alexander, M., Dettori, J. R., Grossman, R. G., Fehlings, M. G., Mirvis, S. E., Shanmuganathan, K., Zacherl, K. M., Burau, K. D., Frankowski, R. F., Toups, E., Shaffrey, C. I., Guest, J. D., Harkema, S. J., Habashi, N. M., Andrews, P., Johnson, M. M., & Rosner, M. K. (2012).Predictors of pulmonary complications in blunt traumatic spinal cord injury. Journal of Neurosurgery: Spine, 17(1 Suppl), 38–45. https://doi.org/10.3171/2012.4.AOSPINE1295
Berlowitz, D. J., Wadsworth, B., & Ross, J. (2016). Respiratory problems and management in people with spinal cord injury. Breathe (Sheff), 12(4), 328–340. https://doi.org/10.1183/20734735.012616
Galeiras Vázquez, R., Rascado Sedes, P., Mourelo Fariña, M., Montoto Marqués, A., & Ferreiro Velasco, M. E. (2013). Respiratory management in the patient with spinal cord injury. BioMed Research International, 2013, Article 168757. https://doi.org/10.1155/2013/168757
Hirota, R., Terashima, Y., Ohnishi, H., Kato, T., Horigome, K., Oichi, T., … & Tanaka, S. (2022). Prognostic factors for respiratory dysfunction for cervical spinal cord injury and/or cervical fractures in elderly patients: A multicenter survey. Global Spine Journal, 14(1), 101–112. https://doi.org/10.1177/21925682221095470
Sampol, J., González-Viejo, M. Á., Gómez, A., García, L., & Escalada, F. (2020). Predictors of respiratory complications in patients with C5–T5 spinal cord injuries. Spinal Cord, 58, 1249–1254. https://doi.org/10.1038/s41393-020-0506-7
Weppner, J. (2025, January 9). Respiratory impairment in SCI. PM&R KnowledgeNow. https://now.aapmr.org/respiratory-impairment-in-sci/
Wong, S. L., Shem, K., & Crew, J. (2012). Specialized respiratory management for acute cervical spinal cord injury: A retrospective analysis. Topics in Spinal Cord Injury Rehabilitation, 18(4), 283–290. https://doi.org/10.1310/sci1804-283
Yang, X.-x., Huang, Z.-q., Li, Z.-h., Ren, D.-f., & Tang, J.-g. (2017). Risk factors and the surgery affection of respiratory complication and its mortality after acute traumatic cervical spinal cord injury. Medicine, 96(36), e7887. https://doi.org/10.1097/MD.0000000000007887