Secretion management
A spinal cord injury (SCI) with a neurological level of injury (NLI) above T12 will result in some degree of respiratory function change. Early assessment will determine predictive factors for respiratory function changes and complications. Frequent monitoring will determine the adequacy of ventilation and sputum clearance, as well as any deterioration in breathing patterns and increase in the work of breathing.
Outcomes will ultimately determine ongoing ventilation and respiratory health needs, depending on the extent of chronic respiratory dysfunction and persistent respiratory risk factors.
Respiratory changes overview
Respiratory changes overview
There are numerous aspects to respiratory function change following an acute spinal cord injury (SCI).
These may include:
- respiratory neuromuscular weakness involving the intercostals, abdominals and possibly even the diaphragm
- reduced diaphragm efficiency due to altered chest wall and abdominal muscle tone and compliance
- restricted inspiratory capacity and decreased forced expiratory volumes and flow rates
- impaired sigh, cough and other forced expiratory actions
- atelectasis and sputum retention
- hypoventilation, which may progress to hypoxaemia and hypercapnia
- increased work of breathing due to altered breathing mechanics—especially in sitting
- increased risk of respiratory fatigue and failure, as well as sleep-disordered breathing.
In summary, these changes collectively lead to reduced ventilation and secretion clearance, along with an increased work of breathing.
For an acute, motor-complete NLI at T6 or above, but especially at C5 and above, significant respiratory function changes occur due to neuromuscular weakness and paralysis, compounded by the presence of spinal shock, as well as autonomic nervous system (ANS) disruption. Key respiratory muscles affected include the intercostal, abdominal and diaphragm muscles.
At this time, weakened or paralysed respiratory muscles present with flaccidity and increased compliance due to spinal shock. This affects diaphragm positioning and function, as well as breathing mechanics. Ultimately, this results in reduced ventilation and secretion clearance. Paradoxical breathing can also develop, which is very inefficient and increases the work of breathing.
For more information on respiratory function changes following SCI, refer to Respiratory changes.
Without adequate and timely intervention, the combination of hypoxaemia, hypercapnia and respiratory fatigue is a key precursor to the onset of respiratory failure. In addition to this, chronic hypoventilation also contributes to sleep-disordered breathing, compounded by any other obstructive and central factors.
During the acute management phase, the following key interventions should be implemented to optimise respiratory management:
• ventilation support
• lung volume augmentation
• secretion management.
These interventions are complementary and should be tailored to the person with SCI’s individual needs.
The role of secretion management
Following SCI, there may be an increased sputum load due to respiratory muscle weakness or paralysis, affecting the ability to generate an effective cough. In addition to this, autonomic nervous system (ANS) disruption can cause an increase in sputum production during the acute phase post-injury, but then again in the context of chronic respiratory dysfunction and ageing.
The combined outcome of any increased sputum load and respiratory muscle impairment is sputum retention. This increases the risk of respiratory complications such as atelectasis and pneumonia, plus failure to wean from ventilation supports.
The primary goals of secretion management are to:
- reduce the viscosity and volume of sputum production, enhancing mucociliary transport
- mobilise sputum from peripheral lung segments to central airways
- expectorate sputum from central airways, stimulating or augmenting a spontaneous and effective cough
- reduce sputum retention
- decreasing atelectasis and airway resistance
- improving alveolar ventilation and lung compliance
- reducing the work of breathing for ventilation
- minimising the colonisation of bacteria and the risk of associated respiratory complications, including pneumonia and long-term bronchiectatic changes
- reducing the degree of hypoventilation during sleep, related to sleep-disordered breathing following SCI
- improve expiratory muscle strength to support
- the process of weaning from ventilation supports
- self-management of secretion clearance
- progression to sitting, engagement in rehabilitation and activities of daily living (ADLs).
Types of secretion management
Overall, a secretion management plan should utilise a range of treatments to address sputum load, viscosity and tenacity for improved clearance using:
- hydration to maintain adequate oral or intravenous cellular hydration (but avoiding pulmonary fluid overload), to reduce mucous viscosity
- humidification to prevent drying of the airway mucosa and mucous (from breathing supplemental oxygen or via ventilation support), to improve the mucociliary transport system as well as reduce mucous viscosity and tenacity
- medications such as
- bronchodilators:
- salbutamol to relax bronchial smooth muscle and improve mucociliary clearance
- ipratropium to inhibit mucous gland activity and cautiously decrease mucous production volume
- mucolytic agents to break down mucous glycoprotein bonds or rehydrate mucous, reducing sputum viscosity and tenacity and enhancing mucociliary clearance
- anti-biotics to reduce the bacterial load and mucous production volume, indirectly reducing sputum viscosity and tenacity and enhancing mucociliary clearance
- bronchodilators:
- invasive ventilation if direct airway access is indicated
- airway clearance techniques (ACTs).
With appropriate medical clearance, appropriate ACTs for a person with SCI should be considered as indicated. Treatment should be delivered by a physiotherapist, or by clinicians and carers, who have been adequately trained by a physiotherapist.
Techniques and devices may be used in combination, along with lung volume augmentation, unless specifically contraindicated or not tolerated. In some cases, lung volume augmentation may need to be repeated at the end of a treatment session, to reverse cough-induced atelectasis. This addresses any airway collapse and re-establishes the functional residual capacity of the lungs for ongoing ventilation.
When using ACTs, the overall approach is to maximise secretion clearance, while minimising treatment-related fatigue for a person with SCI. To support safe and effective delivery, sessions should be conducted efficiently by:
- timing with post bronchodilator and pain relief administration
- managing the energy demand of the treatment
- clustering sessions with personal care tasks to allow deliberate rest periods afterwards.
An overview of ACTs is provided below, including references to recommendations from The Australian and New Zealand Clinical Practice Guidelines: For the Physiotherapy Management of People with Spinal Cord Injury.
The Australian and New Zealand Clinical Practice Guidelines: For the Physiotherapy Management of People with Spinal Cord Injury
Many lung volume augmentation techniques are clinically practised today by physiotherapists. They have evolved over decades, in the treatment of post-surgical and neuromuscular conditions, including SCI. While there is considerable clinical experience in the use of these interventions, there has been limited scientific study of their efficacy in the management of SCI respiratory dysfunction.
In 2022, The Australian and New Zealand Clinical Practice Guidelines: For Physiotherapy Management of People with Spinal Cord Injury were developed, providing evidence-based recommendations where possible, or consensus-based opinion statements.
The process completed systematic reviews and SCI professional peer consultation to address physiotherapy enquiry questions, presented in a PICO (Participant, Intervention, Comparison and Outcome) format. The outcomes are presented as either evidence or consensus statements and form the new clinical practice guidelines. Those which are relevant to the management of respiratory function following SCI, have been incorporated into the “Lung Volume Augmentation” and “Secretion Management” sections. They will be presented using the following colour variations banners.
The Australian and New Zealand Physiotherapy Guidelines for people with SCI states:
Evidence: Weak for recommendation
Guideline
The Australian and New Zealand Physiotherapy Guidelines for people with SCI states:
Consensus: Weak for recommendation
Guideline
The Australian and New Zealand Physiotherapy Guidelines for people with SCI states:
Consensus: Strong for recommendation
Guideline
The Australian and New Zealand Physiotherapy Guidelines for people with SCI states:
Consensus: Weak against recommendation
Guideline
Airway clearance techniques (ACTs)
ACTs can be considered to have two main stages:
- Peripheral ACTs for sputum mobilisation
- Proximal ACTs for cough augmentation.
Peripheral ACTs are utilised before proximal ACTs to reverse atelectasis and improve alveolar ventilation, beginning the process of sputum mobilisation. Peripheral ACTs typically benefit from pre-administration of medications to relax airway bronchospasm and reduce sputum viscosity.
Proximal ACTs are completed after this, to suction or augment cough effort, clearing the upper airway.
Peripheral airway clearance techniques (ACTs)
Lung volume augmentation
As part of peripheral ACTs, lung volume augmentation using a positive-pressure breathing device can be used to treat atelectasis and improve alveolar ventilation, including sputum mobilisation.
This has already been discussed in its own section. For more information, refer to Lung volume augmentation.
Postural drainage
The Australian and New Zealand Physiotherapy Guidelines for people with SCI states:
Consensus: Strong for recommendation
Targeted postural drainage should be provided to improve secretion clearance in people with SCI who have respiratory muscle weakness or paralysis.
Postural drainage is a conventional physiotherapy technique that uses variable body positioning to target sputum mobilisation from specific lung segments, using the influence of gravity and the normal mucociliary action of the lungs. Each position should be maintained for an adequate duration—typically 10-20 minutes per segment—to allow for a physiological effect of sputum transport from peripheral to more central airways.
Postural drainage is usually combined with other ACTs, such as lung volume augmentation, percussion and expiratory vibrations. It may be enhanced by pre-administration of nebulised medications, to improve sputum hydration and viscosity.
If medically permitted and tolerated by the person with SCI, select postural drainage positions may be cautiously introduced in the sub-acute phase of SCI management, to mobilise sputum. It will still be important to monitor and manage the risk of inducing pain and respiratory fatigue while:
- positioning on an appropriate pressure-relieving mattress
- avoiding positions that load areas of skin or tissue breakdown
- closely monitoring repositioning for any adverse impact on ventilation and the work of breathing; for example, sitting upright may increase the work of breathing
- clustering repositioning with other cares, to improve efficiency and allow for adequate rest; also considering that repositioning can be labour-intensive for staff and exhausting for a person with SCI who is acutely unwell.
The following factors will prohibit the safe use of postural drainage:
- unstable spinal fractures or recent spinal surgery
- haemodynamic instability, including arrhythmias, neurogenic shock, pulmonary embolism and autonomic dysreflexia
- thoracic complications, including undrained pneumothorax, tracheoesophageal fistula, haemoptysis, adult respiratory distress syndrome (ARDS).
The following factors will also prohibit trendelenberg (head-down) positioning:
- gastro-oesophageal reflux and any aspiration risk
- heart failure
- conditions with increased/poorly controlled intracranial pressures, including traumatic brain injury.
The following factors will also prohibit upright positioning:
- conditions with increased/poorly controlled intracranial pressures, including traumatic brain injury
- high risk of respiratory fatigue due to significant respiratory muscle weakness and paralysis
- abdominal distension, including paralytic ileus or recent abdominal surgery.
Percussion and expiratory vibrations with compression
The Australian and New Zealand Physiotherapy Guidelines for people with SCI states:
Consensus: Weak for recommendation
Percussion and vibrations may be provided to improve secretion clearance in people with SCI who have respiratory muscle weakness.
Percussion and expiratory vibrations are examples of manual physiotherapy techniques, which are typically combined and interspersed with lung volume augmentation techniques.
Percussion involves rhythmic clapping on the chest wall, using cupped hands. The purpose is to create mechanical vibrations that are transmitted through the chest wall into the tracheobronchial tree, creating shearing forces at the sputum–airway interface to dislodge sputum from the airways. Expiratory vibrations are also a manual chest physiotherapy technique, but involve applying a fine, fast vibration which is progressively, compressive to the chest wall, usually with flat hands during exhalation. These forces are also transmitted through the chest wall into the tracheobronchial tree, while using increased peak expiratory flow to mobilise sputum along the airway during exhalation.
If medically permitted and tolerated by the person, percussion and expiratory vibrations with compression may be cautiously introduced in the sub-acute phase of SCI management, to mobilise sputum. It will still be important to monitor and manage the risk of inducing pain and respiratory fatigue.
The following factors will prohibit the safe use of percussions and expiratory vibrations with compressions:
- abdominal distension, including paralytic ileus or recent abdominal surgery
- unstable spinal fractures or recent spinal surgery
- gastro-oesophageal reflux and any aspiration risk
- haemodynamic instability, including arrhythmias, neurogenic shock, pulmonary embolism and autonomic dysreflexia
- thoracic complications, including sternal/rib fractures, osteoporosis, undrained pneumothorax, tracheoesophageal fistula, haemoptysis, adult respiratory distress syndrome (ARDS).
The following alternative forms of peripheral ACTs are discussed and their potential application for sputum mobilisation in SCI management.
Intrapulmonary percussive ventilation (IPV) devices
Intrapulmonary percussive ventilation (IPV) devices
Intrapulmonary Percussive Ventilation (IPV) devices deliver aerosolised medication, to address sputum hydration and viscosity, via high-frequency bursts of low-pressure gas—typically 100-300 cycles per minute. This creates oscillating inspiratory and expiratory airway pressures, ranging from 10-40 cmH₂O. This expands the lungs and internally vibrates and dilates the peripheral airways—similar to the external technique of percussion—for the purpose of dislodging sputum.
For the user, it may enable a more efficient, consistent and customised experience in comparison to the traditional manual therapy. For therapists and carers, it may reduce the manual handling risks associated with repetitive strain injuries.
IPV has been more commonly used in the treatment of chronic pulmonary diseases, including cystic fibrosis and bronchiectasis, as well as degenerative neuromuscular conditions. However, some mechanical insufflation exsufflation (MI-E) devices used in SCI respiratory management, are now providing the addition feature of IPV, called a “Percussor mode”. This effectively broadens the scope of the MI-E device to provide sputum mobilisation (peripheral ACT), in addition to its familiar role in lung volume and cough augmentation (proximal ACT).
Available interfaces include mouthpiece and face mask, with some also permitting attachment to tracheostomy and endotracheal tubes. However, similar to MI-E devices offering burst NIV and IPPB modes, the attached circuit is required to have an expiratory valve/leak port to prevent CO₂ rebreathing during longer use (disconnect user from MI-E device when treatment is complete).
- Some circuits have a switch valve on the circuit to open or close when changing between modes (MI-E mode (closed) and IPPB, NIV, IPV (open)).
- Some circuits have the exhalation valve/leak port as an extra attachment (it is normally preferable to operate with 2 circuits: 1 circuit dedicated to MI-E and another circuit dedicated to the other modes)
Given IPV can generate high frequency and airway pressures, cautious clinical introduction would be important, to minimise the risk of barotrauma in the acute phase of SCI management or when introducing to a person with a chronic SCI who has reduced airway and chest wall compliance.
More time is needed to determine the clinical utility of this feature for sputum mobilisation in SCI respiratory management, including how to optimise the provided parameters e.g. inspiratory pressure (e.g. 0-70 cmH20), frequency (e.g. 10-780 CPM) and the inspiratory to expiratory ratio (typically ranging 1:5 to 5:1).
However, a clinical trial of IPV, may otherwise be appropriate in the acute and chronic phase of SCI management:
- if there is a high sputum load and MI-E is not being effective on its own
- to reduce therapist and carer manual handling and the risk of repetitive strain injuries, related to percussion
- if percussion is otherwise not tolerated, but also not contraindicated.
Oscillation and compression (HFCWO and HFCWC) devices
Oscillation and compression (HFCWO and HFCWC) devices
There are other distinct therapies which provide chest wall vibration and oscillations, via unique devices. This includes high frequency chest wall oscillations (HFCWO) and high frequency chest wall compression (HFCWC). Using inflatable chest vests and wraps which are externally applied, it generates an external vibration with compression—similar to the external technique of expiratory vibrations with compression—for the purpose of dislodging sputum.
For the user, it may enable a more efficient, consistent and customised experience in comparison to the traditional manual therapy. For therapists and carers, it may reduce the manual handling risks associated with repetitive strain injuries.
While again not commonly used for sputum mobilisation in SCI respiratory management, some MI-E devices are now providing accessory options which provide additional features referred to as HFCWO (along with HFCWC). Similar to IPV, this effectively broadens the scope of the MI-E device to provide sputum mobilisation (peripheral ACT), in addition to its familiar role in lung volume and cough augmentation (proximal ACT).
Newer designs favour use of an inflatable wrap, and this may also be easier to apply when an adult user is supine.
Inclusion of HFCWO would not be considered appropriate during the acute phase of SCI management, when a person is ventilator dependent, has unstable spinal and chest wall injuries, significant pain or at high risk of respiratory fatigue. It would also not be appropriate if there were concerns regarding risk of spinal or chest wall fracture in a person with a chronic SCI.
More time is needed to determine the clinical utility of this accessory for sputum mobilisation in SCI respiratory management, including how to optimise the provided parameters e.g. oscillations (e.g. 50-900 bpm/0.83-15Hz), compression (e.g. 5-70cm H20) and the inspiratory to expiratory ratio (typically 1:1). In addition to this, while NIV support is commonly provided when HFWCO is used in paediatric populations with neuromuscular disease, it is unknown if ventilation support may be required in adult populations with SCI. Issues such as the increased work of breathing and altered lung/chest wall compliance following SCI in the acute versus chronic stage post-injury will be important to address.
However, a clinical trial of MI-E with the addition of HFCWO, may otherwise be appropriate in the sub-acute and chronic phase of SCI management:
- if there is a high sputum load and MI-E is not being effective on its own
- to reduce therapist and carer manual handling and the risk of repetitive strain injuries, related to expiratory vibrations with compression.
Positive expiratory pressure (PEP) devices
Positive expiratory pressure (PEP) devices
The Australian and New Zealand Physiotherapy Guidelines for people with SCI states:
Consensus: Weak against recommendation
Positive expiratory pressure devices should not be provided to improve secretion clearance in people with SCI who have expiratory muscle weakness.
Positive expiratory pressure (PEP) therapy can be delivered using a handheld device or integrated into an inspiratory muscle trainer. It may also be combined with a nebuliser or connected in-line with a mechanical ventilator circuit. Varied inspiratory lung volumes are used to apply forceful, sustained exhalation against a fixed or oscillating resistance pressure—typically between 10-20 cmH₂O.
PEP generates a positive pressure within the lungs and splints open the airways during the expiratory phase of breathing. It aims to improve alveolar collateral ventilation, while enhancing functional residual capacity and minimising dynamic airway collapse during forced exhalation.
PEP therapy is more commonly used in the treatment of chronic pulmonary diseases, including cystic fibrosis and bronchiectasis, rather than sputum mobilisation in SCI respiratory management.
In the presence of significant respiratory muscle weakness following SCI, the technique is very difficult to perform effectively. There is also a heightened risk of creating barotrauma, worsening hypercapnia or exacerbating respiratory fatigue for a person in the acute phase of SCI management.
For these reasons, the use of PEP is not recommended as a peripheral ACT for a person with SCI, who has expiratory muscle weakness during acute management.
However, if respiratory muscle function improves, PEP therapy may otherwise be appropriate in the sub-acute and chronic phase of SCI management where:
- the risk of respiratory fatigue is minimal
- there is a high sputum load and risk of airway collapse
- the user has some degree of expiratory muscle function and is appropriate to commence expiratory muscle training.
Autogenic drainage (AD) technique
Autogenic drainage (AD) technique
Similar to the effect of chest wall strapping (CWS), autogenic drainage (AD) uses the effect of expiratory flow at low lung volumes. AD does not use a device. Rather it requires a range of inspiratory lung volumes to be achieved, followed by varying forced expiratory flow rates, across three distinct stages of breathing. By generating different exhalation pressures, autogenic drainage mobilises sputum from small peripheral airways, toward larger central airways—while also minimising dynamic airway collapse during exhalation.
Effective performance requires coaching, along with a sufficiently high sputum load to provide the necessary auditory feedback to the user. It also requires significant and sustained expiratory muscle control.
Because AD involves repeated inspiratory efforts and forced exhalations, it is likely to become fatiguing for a person with an acute SCI. Significant respiratory muscle weakness also makes this technique difficult to perform effectively.
AD breathing techniques are more commonly used in the treatment of chronic pulmonary diseases, including cystic fibrosis and bronchiectasis, rather than SCI respiratory management.
However, if respiratory muscle function is adequate, AD breathing may otherwise be appropriate in the sub-acute and chronic phase of SCI management where:
- the risk of respiratory fatigue is minimal
- there is a high sputum load and risk of airway collapse
- the user has some degree of expiratory muscle function and is able to respond to the necessary coaching.
Proximal airway clearance techniques (ACTs)
Given the significant risk of respiratory fatigue, most of the treatment time should focus on adequately mobilising secretions from the peripheral to the central airways using: hydration, humidification, medications, ventilatory support, lung volume augmentation, and peripheral ACTs as discussed above.
When secretions become audible or palpable in the upper airways, proximal ACTs should be introduced to facilitate clearance but not be excessively used due to the risk of respiratory fatigue.
Clinicians and carers should use appropriate personal protective equipment (PPE) when managing secretions and airborne particles—for example, eye goggles or face shield, face mask, and gloves.
Tracheal suctioning
This sterile technique is used when invasive ventilation support is required and there is significant sedation and/or respiratory muscle weakness and paralysis. It provides secretion removal via a suction catheter passed through an invasive airway to a level just above the bifurcation of the trachea.
The effectiveness of suctioning is limited to the suction catheter reach, plus the degree of reflexive cough triggered.
Hence, it will have limited forced expiratory volume or flow rate due to:
- no immediate increase in lung volume prior to the reflexive cough
- impeded glottal function due to an endotracheal tube or cuffed tracheostomy tube
- respiratory muscle weakness and paralysis.
Other forms of proximal ACTs should be introduced when appropriate, specifically cough augmentation strategies.
Cough augmentation strategies
Cough augmentation strategies are used to assist the action of weakened or paralysed expiratory muscles, required for effective coughing. This helps improve expiratory volume and flow rate for enhanced sputum clearance, while reducing the risk of respiratory fatigue.
If medically permitted and tolerated by the person with SCI, cough augmentation may be introduced to assist sputum clearance, while considering:
- cough effectiveness is enhanced by the prior use of lung volume augmentation and peripheral ACTs
- subjective assessment of cough effectiveness may include observations of user tolerance, the degree of chest wall expansion during inspiration, and the force, volume, and productivity of the cough
- objective assessment may involve spirometry to evaluate the
- the cough, without lung volume and cough augmentation (peak cough flow (PCF))
- the cough, with cough augmentation, but without lung volume augmentation (PCFassisted))
- the cough, with lung volume augmentation and cough augmentation (PCFassisted).
Spirometry indicators for cough augmentation.
PCF < 270 L/min indicates reduction in lung volumes and respiratory muscle strength: there is a high risk of developing retained secretions—use of lung volume augmentation as well as manual assist cough may be indicated. Use of a mechanical assisted cough device may be preferable if there is a high risk of respiratory fatigue and further respiratory deterioration.
PCF < 160 L/min indicates significant reduction in lung volumes and respiratory muscle strength: there is a high risk of developing retained secretions, even with a manual assisted cough—use of lung volume augmentation as well as mechanical assisted may be indicated. A manual assisted cough may be added in addition to this.
MEP < 60 cmH20 indicates significant reduction in expiratory muscle strength: cough is ineffective and there is a high risk of developing retained secretions, even with a manual assisted cough—use of ventilation support, lung volume augmentation as well as mechanical +/- manual assisted cough may be indicated.
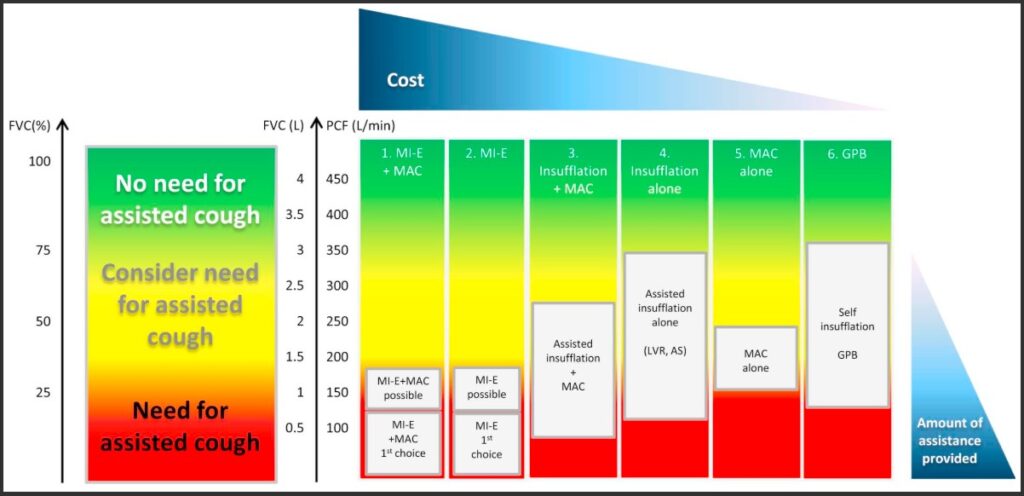
Graph of spirometry indicators for lung volume augmentation and cough augmentation in neuromuscular disorders
Toussaint, M., Chatwin, M., González, J., Berlowitz, D. J., & ENMC Respiratory Therapy Consortium. (2018). 228th ENMC International Workshop: Airway clearance techniques in neuromuscular disorders, Naarden, The Netherlands, 3–5 March, 2017. Neuromuscular Disorders, 28(3), 289–298. https://dhttps://doi.org/10.https://www.nmd-journal.com/article/S0960-8966(17)30588-6/fulltext#f00101016/j.nmd.2017.10.008
Mechanical insufflation-exsufflation (MI-E)
The Australian and New Zealand Physiotherapy Guidelines for people with SCI states:
Consensus: Strong for recommendation
Mechanically assisted cough (insufflation-exsufflation) should be provided to improve secretion clearance in people with SCI who have abdominal muscle weakness or paralysis and an ineffective cough.
Mechanical Insufflation-Exsufflation (MI-E) device
Adapted from SCIRE Professional
Although first developed during the polio epidemic, mechanical insufflation-exsufflation (MI-E) technology has since evolved and is now commonly referred to as a “Cough Assist” device.
MI-E devices provide both lung volume augmentation (insufflation = inspiration) and cough augmentation (exsufflation = forced expiration). These two modes are complementary—by increasing inspiratory volume, expiratory flow and volume are also enhanced, leading to improved cough effectiveness.
MI-E therapy does not require the user to be able to breathe spontaneously or cooperate, so it can be cautiously introduced with invasive ventilation. However, if available, use of any ventilator hyperinflation setting is initially preferable to reduce the risk of volutrauma/barotrauma before introducing MI-E therapy. However, MI-E therapy is certainly advantageous to introduce prior to, during and after any weaning for extubation/decannulation.
MI-E devices may provide single breaths, with some also permitting stepped insufflations. Either way, it can be used to achieve maximal insufflation capacity (MIC) and reduce the associated work of this breathing. While most devices do not provide expiratory positive airway pressure (EPAP) during exhalation, all MI-E devices provide exsufflation.
Pre-programming MI-E treatment sessions allows lung volume and cough augmentation to be standardised and delivered throughout a 24-hour period by trained non-physiotherapy staff, such as nursing staff, carers, or family members. However, specific training is essential to ensure safe and effective use.
Using a single device, MI-E therapy enables both lung volume and cough augmentation, with their associated respiratory benefits. As the work of breathing for both is significantly reduced, treatment is less likely to contribute to respiratory fatigue during acute management.
MI-E method
- The MI-E device uses compressed air +/- oxygen and is typically pressure-controlled, but time-cycled.
- The operator sets various parameters including whether treatment will be insufflation +/- exsufflation, as well as the maximum pressures and time for insufflation +/- exsufflation, the insufflation flow rate or rise time and inspiratory trigger sensitivity.
- The operator initiates mechanical insufflation using the device toggle switch (on the device, hand remote or foot pedal) via an appropriate circuit and interface attached to the user.
- A positive pressure breath is delivered by the device (typically 20 to 40 cmH₂O), up to the user’s maximal insufflation capacity (MIC). This supports lung volume augmentation with minimal effort from the user.
- Expiration occurs passively through the attached circuit with nil exhalation valve/leak port (unless using the following other non-MI-E modes on the same device).
- A series of insufflation breaths is delivered for lung volume augmentation and sputum mobilisation; a mechanical assisted cough can then be triggered by rapidly reversing airflow to generate negative pressure (typically –20 to –40 cm H₂O). This sudden shift in pressure simulates a cough, without requiring active effort from the user. The effectiveness of the cough is enhanced by increasing the pressure gradient between insufflation and exsufflation, thereby increasing forced tidal volume and peak expiratory flow. A manual assisted cough (MAC) can be applied simultaneously to further improve cough effectiveness.
- While optimal MI-E dosage and frequency has not been determined yet, a typical MI-E treatment session may be repeated cycles of 3 pre-therapy breaths, 2 exsufflations, 2 post-therapy breaths. Other treatment approaches may consist of cycling between insufflation and exsufflation, with a exsufflation cough as needed.
MI-E variations
Modes may include:
- manual– allows the operator greater control over insufflation and exsufflation timing and pressures
- automatic– enables pre-programmed cycle for consistent, repeatable therapy—suitable for unsupervised use by trained clinicians and carers
- IPPB– supports programmed lung volume recruitment initiated by the user when needed
- burst NIV– provides EPAP typically used before or after treatment for respiratory rest, while maintaining any lung volume recruitment; it is not intended for continuous ventilatory support and will be time limited e.g. <15 minutes; it is not for users with a tracheostomy or endotracheal tube
- Intrapulmonary Percussive Ventilation (IPV) or “Percussor Mode”– provides airway percussion therapy with settings for frequency (e.g. 10-780 CPM), pressure (e.g. 0-70 cmH20) and I:E ratios (e.g. 1:5 to 5:1)
- High Frequency Chest Wall Oscillations (HFCWO)– typically using an inflatable chest wrap to provide external chest wall percussion with settings for frequency (e.g. 50-900 bpm), pressure (e.g. 5-70 cmH20) and I:E ratios (typically 1:1).
Circuit design must be appropriate to the mode, as well as the actual device.
- Most MI-E devices use a single lumen circuit, although dual lumen may be required, ensuring there is no contamination between insufflation and exsufflation debris
- Manual and automatic MI-E modes use standard MI-E circuits which have no exhalation valve/leak ports, to allow for delivery of negative pressure delivered in short treatment sessions (disconnect user from MI-E device when each short treatment session is complete)
- In contrast, IPPB, NIV and IPV modes require a circuit with an exhalation valve/leak port, to prevent CO₂ rebreathing during longer use (disconnect user from MI-E device when treatment is complete).
- Some circuits have the exhalation valve/leak port as an extra attachment (it is normally preferable to operate with 2 circuits: 1 circuit dedicated to MI-E and another circuit dedicated to the other modes)
- Some circuits have a switch valve on the circuit to open or close when changing between modes (MI-E mode (closed) and IPPB, NIV, IPV (open)).
Additional features may include:
- interface options such as a non-vented mask (preferred) versus mouthpiece, and sometimes a tracheostomy or endotracheal tube connector
- options for ambient air, and sometimes supplemental oxygen via an entrainment port and/or humidification
- recorded measures of volume and exsufflation flow rate, pulse oximetry for monitoring during treatment sessions
- real time pressure wave and bar graphs for feedback during treatment sessions
- real time capacity to record or adjust treatment sessions
- parameter variations may include
- insufflation and exsufflation pressures and time ratios, with some providing an option for stepped insufflation
- pause time between insufflation and exsufflation/cough
- flow rate or rise time options for each insufflation
- sensitivity trigger options for insufflation
- synchrony options for insufflation or exsufflation/cough
- airway oscillations on insufflation, exsufflation or both with a selection range for frequency (e.g. 4-20 Hz) and amplitude (e.g. 1-10 cmH20)
- EPAP on pause breath
- options for pre-therapy and post-recruitment breaths
- number of pre-save programs for different types of therapies, including when well and unwell.
Additional accessories may include:
- option of a stand as well as mask holders
- internal battery (e.g. 3-4 hr capacity) in addition to external power supply
- hand remote or foot pedal
- pulse oximeter.
Additional variations may include:
- overall weight of device
- device handle, carry bag etc.
- customisation of screen colours, or orientation of screen for visualisation
- touch screen versus button operation, including varying sensitivity and ease of navigation
- connectivity e.g. ethernet, USB, USB C, HDMI port, flash drive, wifi, bluetooth
- remote control access e.g. app to adjust device settings via a mobile phone
- data download processes i.e. simple vs multi-stage
- access to compliance summary/user log
- safety prompts about correct circuit +/- external valve/leak port
- terminology and use of positive (+) and negative (-) numbers for insufflation and exsufflation
- provision of user quick reference guides and online resources.
MI-E clinical reasoning
Recommendations for use include:
- during the initial use of MI-E carefully monitor oxygen and heart rate settings to ensure safety; if there is a high sputum load, it may be advisable to have suction and resuscitation equipment ready
- start pressure settings low and seek user feedback, while monitoring chest wall expansion to determine adequacy of pressure settings; typically start insufflation with 15 cmH20 and increase in 5 cmH20 increments (unless the user is also accessing NIV, then start insufflation NIV IPAP +5 cmH20 and increase in 5 cmH20 increments)
- keep exsufflation pressure 5-10 cmH20 more negative than insufflation pressure to maintain a pressure gradient that biases sputum mobilisation
- progressively increase pressures until efficacy is achieved, remembering the delivered tidal volume varies depending on airway resistance, lung compliance, and circuit integrity
- individually adjust inspiratory and expiratory time/rise/pressures for each user, matching their normal breathing pattern and optimising comfort
- if adding oscillations, adjust insufflation and exsufflations pressures to factor in the additional pressure overlay; however, there is little evidence this is a useful feature when compared to options with percussor modes
- if there are concerns about chest wall and spine bone mineral density, or chest wall and lung compliance, start with lower flow rates and pressures; also opt for IPV mode rather than use HFCWO
- measures of volume and peak flow rate are not always accurate and represent gas decompression in the device circuit, so also compare to pressure-wave forms as well as observations of the chest wall and sound of the cough effectiveness
- when the user is spontaneously breathing, use of a non-vented face mask is preferable to a mouthpiece
- MI-E use may be an option for ventilated users, but extreme caution is required to reduce the risk of volutrauma/barotrauma. In these cases:
- it may be safer to leave the invasive airway cuff deflated and permit some leakage, rather than inflating to maximise pressure delivery to the lung periphery
- inspiratory pressure settings may need to be carefully increased to account for increased airway resistance, dead space and leakage.
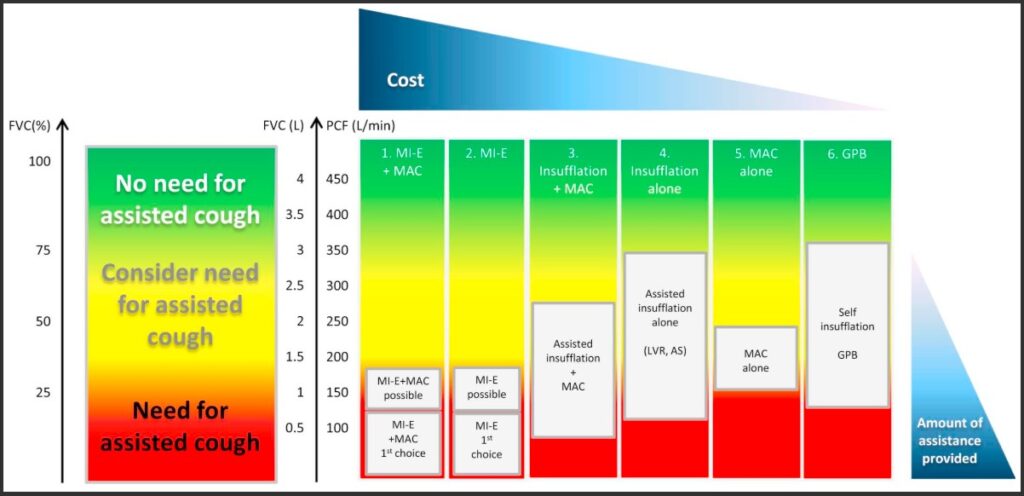
Graph of spirometry indicators for lung volume augmentation and cough augmentation in neuromuscular disorders
Toussaint, M., Chatwin, M., González, J., Berlowitz, D. J., & ENMC Respiratory Therapy Consortium. (2018). 228th ENMC International Workshop: Airway clearance techniques in neuromuscular disorders, Naarden, The Netherlands, 3–5 March, 2017. Neuromuscular Disorders, 28(3), 289–298. https://dhttps://doi.org/10.https://www.nmd-journal.com/article/S0960-8966(17)30588-6/fulltext#f00101016/j.nmd.2017.10.008
The following are examples of published flowcharts for the safe introduction and titration of basic MI-E parameters in adults with neuromuscular disease, including SCI. It is also important to note that device pressure and volume readings may not accurately indicate the lung volume augmentation or peak cough flow achieved. Rather subjective reports from the user and objective assessment of chest wall expansion and the sound of the cough should also inform titration.
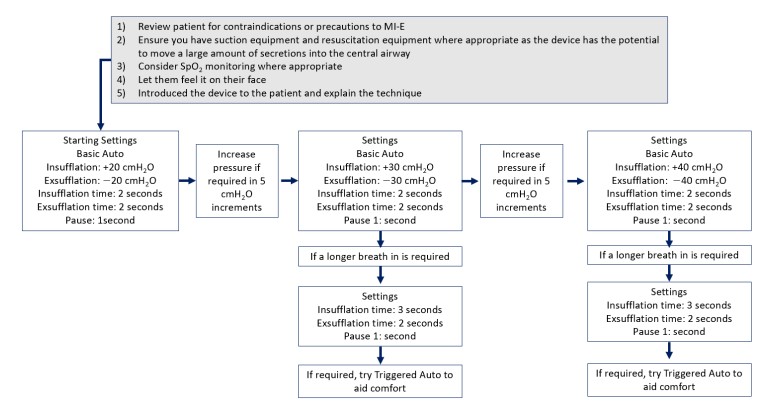
Flowchart for a standard approach to initiation of MI-E in adults
Chatwin, M., & Wakeman, R. H. (2023). Mechanical Insufflation-Exsufflation: Considerations for improving clinical practice. Journal of Clinical Medicine, 12(7), Article 2626. https://doi.org/10.3390/jcm12072626
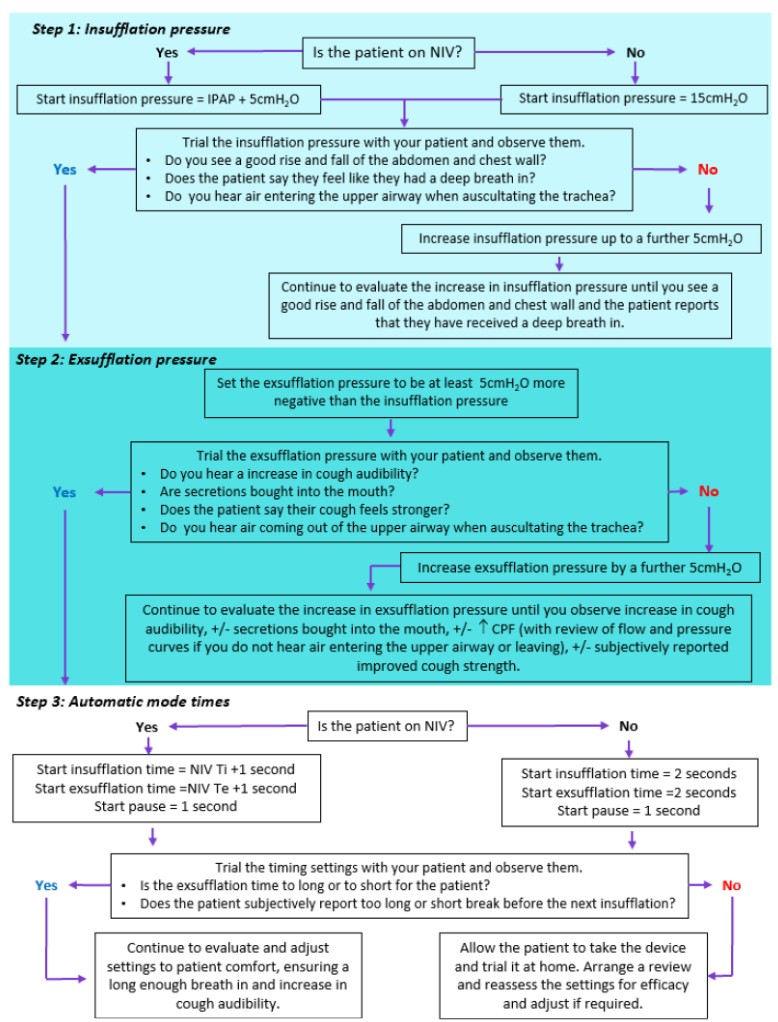
Flowchart for a personalised approach to titration of MI-E in adults
Chatwin, M., & Wakeman, R. H. (2023). Mechanical Insufflation-Exsufflation: Considerations for improving clinical practice. Journal of Clinical Medicine, 12(7), Article 2626. https://doi.org/10.3390/jcm12072626
MI-E video information
MI-E more information
More information about MI-E can be found here.
In addition to factors which prohibit the safe use of positive-pressure breathing devices, the following also prohibits the safe use of MI-E devices:
- drained pneumothorax- due to negative exsufflation pressures
- unconscious- due to lack of user feedback.
Manual assisted cough (MAC)
The Australian and New Zealand Physiotherapy Guidelines for people with SCI states:
Consensus: Strong for recommendation
Manually assisted cough should be provided to improve secretion clearance in people with SCI who have abdominal muscle weakness or paralysis and an ineffective cough.

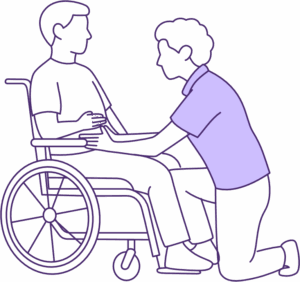
Manual assisted cough (MAC) techniques for a person with SCI in supine lying and sitting
Image source: QSCIS
A manual assisted cough (MAC) is best performed when the user is able to breathe spontaneously or cooperate, to maximise cough effectiveness.
Also referred to as a “quad cough,” a MAC involves coordinated effort, between the person with SCI and the operator.
However, the MAC technique can be cautiously introduced with mechanical ventilation, to time with suctioning or use of a mechanical insufflation/exsufflation (MI-E) device. It is an important technique to introduce, before commencing weaning and decannulation of ventilation supports.
A MAC can be completed by trained non-physiotherapy staff, such as nursing staff, carers, or family members. However, specific training is essential to ensure safe and effective use. It can be a version of the Heimlich manoeuvre or use variations of abdominal thrusts and costophrenic/chest wall compressions to achieve. The technique selected, will determine the direction of the manual force required—it must be consistent with the mechanics of exhalation and flow of expiratory air.
Considerations include that the MAC:
- requires formal training to be performed safely and with appropriate ergonomics, although the risk of repetitive strain injury (RSI) remains
- can be staffing-intensive when more than one clinician is required for repeated use—in such cases, the use of a MI-E device is recommended when available
- may be performed in a variety of positions, including lying or sitting; when the user is seated in a manual wheelchair, ensure the wheelchair is backed against a wall/second person or secured to prevent tipping backward during the MAC thrust and that the user’s head is protected with a headrest or pillow
- may be used as an emergency intervention in the event of choking.
MAC method
The MAC technique requires the operator to have CORRECT hand positioning, directional force, co-ordination and cueing.
A variety of hand or forearm positions can be utilised, typically with a thrust given at the abdomen +/- compression on the chest wall.
The number of operators may vary from 1 to 3, depending on the needs and size of the person with SCI.
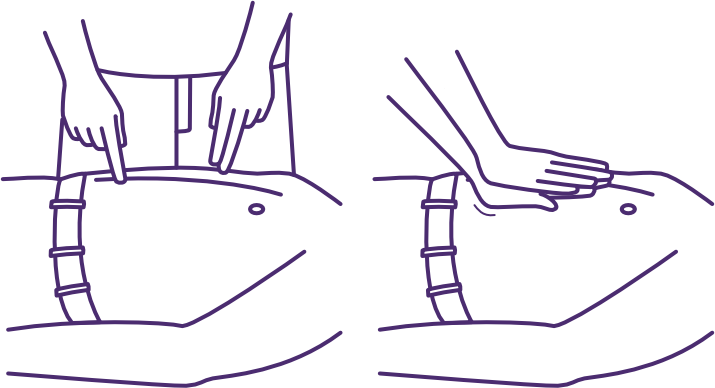
Manual assisted cough (MAC) hand positioning on upper abdomen
Image source: QSCIS
| Hand/forearm positioning | Thrust is applied by positioning hands/forearms on the upper abdomen, above the naval but below the base of the sternum. Additional compression can also be applied by positioning hands/forearms across the anterior or lateral chest wall. | |
| Force direction | Thrust direction is up towards the person with SCI’s tracheostomy/mouth. Compression direction is to cause deflation of the rib cage. | |
| Co-ordinated timing | The operator should verbally ‘coach’ the whole process but follow the ‘cues’ of the person with SCI e.g. readiness, comprehension using observation and palpation of the respiratory cycle Note a person with SCI’s abdomen -will rise during inspiration -will fall during expiration/cough attempt. Before the cough, a series of deep breaths is recommended to maximise inspiratory volume and therefore, expiratory volume and flow rate. Prior air stacking with an LVR bag etc. may also be useful to augment lung volumes. At the end of the final deep breath, the thrust +/- compression given by the operator must occur at the same time as the person with SCI’s reflexive/voluntary cough. | |
| Cueing script example | NO LVR BAG “I’m going to help you cough after you take 3 deep breaths: Breathe in, breath out: that’s # 1 Breathe in, breath out: that’s # 2 Breathe in, hold: now COUGH!” | WITH LVR BAG and 1 operator “Take your deepest breath on your own. HOLD. Now put your mouth around the LVR mouthpiece and let me squeeze more air into your lungs until you give me the cue to stop. HOLD Now remove your mouth from the mouthpiece. HOLD. Now COUGH!” |
MAC video demonstrations
MAC more information
More information about MAC can be found here.
The following factors will prohibit the safe use of a MAC technique:
- pregnancy
- abdominal distension, including paralytic ileus or recent abdominal surgery
- recent food intake (within 1.5 to 2 hours, although chest wall compression may be permitted)
- reduced airway protection, including bulbar dysfunction, gastro-oesophageal reflux or any increased aspiration risk
- risk of inducing fatigue due to prolonged respiratory treatments, including repeated coughing efforts
- unstable spinal fractures or recent spinal surgery
- fractured sternum/ribs, osteoporosis
- poorly controlled intracranial pressures
- severe facial injuries
- haemodynamic instability, including arrhythmias, neurogenic shock, pulmonary embolism and autonomic dysreflexia
- thoracic complications, including undrained pneumothorax, tracheoesophageal fistula, haemoptysis, adult respiratory distress syndrome (ARDS).
Combined MI-E and MAC
The Australian and New Zealand Physiotherapy Guidelines for people with SCI states:
Consensus: Strong for recommendation
A combination of mechanically assisted cough and manually assisted cough should be provided to improve secretion clearance in people with SCI who have abdominal muscle weakness or paralysis and an ineffective cough.
To maximise cough effectiveness and minimise the risk of respiratory fatigue, it is considered best practice to combine both cough augmentation strategies:
- mechanical insufflation-exsufflation (MI-E) device, if available
- manual assisted cough (MAC) technique, if tolerated.
MI-E + MAC video demonstration
A video demonstrating MI-E + MAC therapy is here.
Abdominal binder
The Australian and New Zealand Physiotherapy Guidelines for people with SCI states:
Consensus: Weak for recommendation
Abdominal binder may be provided to improve cough in people with SCI who have abdominal muscle weakness or paralysis.
Abdominal binders (to improve cough) are provided in people with abdominal paralysis (partial or full) and may not be suitable for people significant abdominal distension, central adiposity or large abdomens. Abdominal binders may also be provided for purposes other than improving cough.
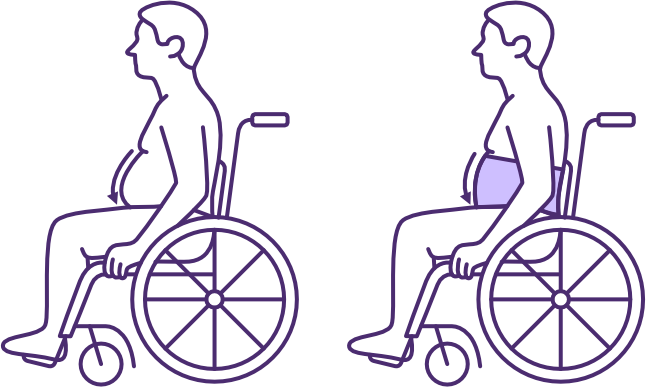
Effect of an abdominal binder on abdominal compliance in sitting following high-level SCI
Image source: QSCIS
If abdominal muscle paralysis or significant weakness is present, the use of an abdominal binder is recommended when sitting—and possibly standing.
A well-fitted abdominal binder helps counteract the loss of normal abdominal muscle tone and increased abdominal compliance, when changing position from supine (where gravity is providing positional assistance). It applies pressure across the abdomen onto the abdominal contents to support:
- venous return in the inferior vena cava, to maintain blood pressure
- dome-shaping of the diaphragm, to improve its position for efficient contraction
- passive and forced expiration.
Overall, the abdominal binder is clinically used in the management of orthostatic hypotension, along with the use of compression stockings and pharmacological interventions.
Due to respiratory changes following SCI, the abdominal binder is also used to enhance lung volumes and reduce the work of breathing in sitting, while improving coughing. One study reported that use of an abdominal binder in sitting for people with a complete SCI above T1, improved maximal inspiratory pressure (MIP), vital capacity (VC), forced expiratory volume in 1 second (FEV1) and peak expiratory flow (PEF). It also increased the time for sustained voice.
Anecdotal evidence suggests that an abdominal binder may also assist with balance and postural cueing during early rehabilitation.
Expiratory muscle training (EMT)
The Australian and New Zealand Physiotherapy Guidelines for people with SCI states:
Evidence: Weak for recommendation
Respiratory muscle training may be used to improve respiratory muscle strength in people with SCI who have respiratory muscle weakness.
Respiratory muscle training most commonly involves inspiratory muscle training but can also include expiratory muscle training
Inspiratory muscle training (IMT) aims to improve diaphragm function, increase tidal and inspiratory reserve volumes, augment expiratory volumes and enhance postural stability while maintaining ventilation.
Expiratory muscle training (EMT) aims to improve the strength of weakened (not paralysed) expiratory muscles to:
- improve diaphragm positioning, via the abdominal contents supporting the diaphragm shape at rest and during contraction
- increase expiratory flow rates and volumes, via intra-abdominal pressure generation
- enhance posture, core stability and trunk function, via abdominal muscle control.
To guide the development of an EMT program, it is useful to:
- identify the acute and chronic respiratory goals: EMT may
- facilitate readiness for weaning and decannulation by
- reducing the risk of respiratory fatigue related to the increased work of breathing from
- poor diaphragm positioning for inspiration, especially in sitting
- weakened abdominal power for coughing
- enhancing the effectiveness of cough for sputum clearance and therefore, reducing the risk of respiratory complications
- reducing the risk of respiratory fatigue related to the increased work of breathing from
- enhance posture, core stability and trunk function, while maintaining ventilation in sitting or standing
- build expiratory capacity and reserve for
- speech volume and phrase length
- engagement in rehabilitation
- activities of daily living etc.
- chronic periods of ill health or confinement to bed
- slow respiratory function decline which is associated with chronic SCI and ageing.
- facilitate readiness for weaning and decannulation by
- identify the key respiratory muscles and types of exercises/activities: EMT may target
- strengthening the abdominal, internal intercostals and expiratory accessory muscles
- for explosive expiratory actions such as coughing and sneezing
- for sustained and coordinated expiratory actions such as blowing (e.g. appropriate use of positive expiratory pressure PEP devices), huffing, speaking in longer phrases, or singing
- for core stability tasks
- complementary stretching of the trunk and associated chest wall, including use of positive-pressure breathing devices to also improve lung and chest wall compliance
- strengthening the abdominal, internal intercostals and expiratory accessory muscles
- identify the type of training effect: EMT could incorporate
- resistance training via high intensity contractions with few repetitions
- endurance training via low-intensity contractions, repeated or held over an extended period of time
- specific exercises versus activity specific tasks and training approaches
- complementary stretching
- identify useful baseline measures: EMT could utilise
- spirometry, such as maximal expiratory pressure (MEP), functional vital capacity (FVC) and peak cough flow (PCF)
- other measures e.g. need for cough augmentation during 24-hours, Borg RPE scale, speech and balance measures.
Functional electrical stimulation (FES)
The Australian and New Zealand Physiotherapy Guidelines for people with SCI states:
Consensus: Weak for recommendation
Abdominal FES may be provided to improve stimulated cough in people with SCI who have abdominal muscle paralysis or weakness.
Functional electrical stimulation (FES) may be trialled to recruit weakened muscles or elicit contractions in fully paralysed muscle groups. Achievement of a muscle contraction depends on the presence of an intact spinal reflex arc—therefore, FES is only suitable in cases of upper motor neuron lesions, typically those with a neurological level of injury (NLI) above T12.
To assist with coughing, FES may be applied via surface electrodes positioned over the motor points of the abdominal muscles.
Standard precautions and contraindications for FES use apply and should be reviewed prior to application.
If trialled, abdominal FES for cough stimulation should be evaluated using both subjective and objective measures.
FES of the abdominal muscles for cough augmentation is
- more clinically effective in cases of muscle weakness, rather than complete paralysis, as a biofeedback and/or training effect may be achieved through repeated use
- not often practical in cases of full muscle paralysis, as it requires long-term application of electrodes which may result in skin breakdown and careful placement for FES success; it may be worth trialling in cases where MI-E devices are not an option and a MAC is not tolerated or safe e.g. colostomy, syrinx.
Discharge and community planning
A person with SCI who has ongoing and significant respiratory dysfunction, will require ongoing ventilation and respiratory health supports for community living. Hospital discharge planning processes will need to address funding, care recruitment and training, as well as establish an adequate network of health professional support. A comprehensive process of trialling and scripting will also be important to supply necessary respiratory equipment and consumables.
For further information, refer to Discharge and community planning.
Physiotherapy management of people with spinal cord injury (2022)
The Australian and New Zealand Physiotherapy Guidelines for people with SCI
Respiratory education modules and YouTube channel
Canadian Alternatives in Noninvasive Ventilation (CANVent)
Cough techniques for individuals with tracheostomy
Tracheostomy Education
Mechanical insufflation-exsufflation (MI-E)
Canadian Alternatives in Noninvasive Ventilation (CANVent)
Cough assist and secretion removal
SCIRE Professional
Gravity assisted drainage
Bronchiectasis Toolbox
Autogenic drainage
Bronchiectasis Toolbox
Autogenic drainage
Physiopedia
Manually assisted cough
Canadian Alternatives in Noninvasive Ventilation (CANVent)
Assisted cough
Shephard Center
Girdle/Abdominal binder
SCIRE Professional
Respiratory muscle training
SCIRE Professional
Abdominal neuromuscular electrical stimulation (NMES)
SCIRE Professional
Brennan, M., McDonnell, M. J., Duignan, N., Gargoum, F., & Rutherford, R. M. (2022). The use of cough peak flow in the assessment of respiratory function in clinical practice: A narrative literature review. Respiratory Medicine, 193, 106740. https://doi.org/10.1016/j.rmed.2022.106740
Brown, R., DiMarco, A. F., Hoit, J. D., & Garshick, E. (2006). Respiratory dysfunction and management in spinal cord injury. Respiratory Care, 51(8), 853-870. https://doi.org/10.4187/respircare.05185
Chatwin, M., Toussaint, M., Gonçalves, M. R., Sheers, N., Mellies, U., Gonzales-Bermejo, J., Sancho, J., Fauroux, B., Andersen, T., Hov, B., Nygren-Bonnier, M., Lacombe, M., Pernet, K., Kampelmacher, M., Devaux, C., Kinnett, K., Sheehan, D., Rao, F., Villanova, M., Berlowitz, D., & Morrow, B. M. (2018). Airway clearance techniques in neuromuscular disorders: A state of the art review. Respiratory Medicine, 136, 98–110. https://doi.org/10.1016/j.rmed.2018.01.012
Chatwin, M., & Wakeman, R. H. (2023). Mechanical insufflation-exsufflation: Considerations for improving clinical practice. Journal of Clinical Medicine, 12(7), 2626. https://doi.org/10.3390/jcm12072626
Galeiras Vázquez, R., Rascado Sedes, P., Mourelo Fariña, M., Montoto Marqués, A., & Ferreiro Velasco, M. E. (2013). Respiratory management in the patient with spinal cord injury. BioMed Research International, 2013, Article 168757. https://doi.org/10.1155/2013/16875
Harvey, L. A. (2008). Management of spinal cord injuries: A guide for physiotherapists. Churchill Livingstone Elsevier.
Reyes, M. R. L., Shaffer, J., Kwong, C., & Gater, D. (2020). A primary care provider’s guide to managing respiratory complications after spinal cord injury. Top Spinal Cord Inj Rehabil, 26(2), 116–124. https://doi.org/10.46292/sci2602-116
Toussaint, M., Chatwin, M., González, J., Berlowitz, D. J., & ENMC Respiratory Therapy Consortium. (2018). 228th ENMC International Workshop: Airway clearance techniques in neuromuscular disorders, Naarden, The Netherlands, 3–5 March, 2017. Neuromuscular Disorders, 28(3), 289–298. https://doi.org/10.1016/j.nmd.2017.10.008
Willis, L. D. (2023). Cough peak flow assessment: Is there more to the story? Respiratory Care, 68(4), 553–555. https://doi.org/10.4187/respcare.10900
Wong, S. L., Shem, K., & Crew, J. (2012). Specialized respiratory management for acute cervical spinal cord injury: A retrospective analysis. Topics in Spinal Cord Injury Rehabilitation, 18(4), 283–290. https://doi.org/10.1310/sci1804-283