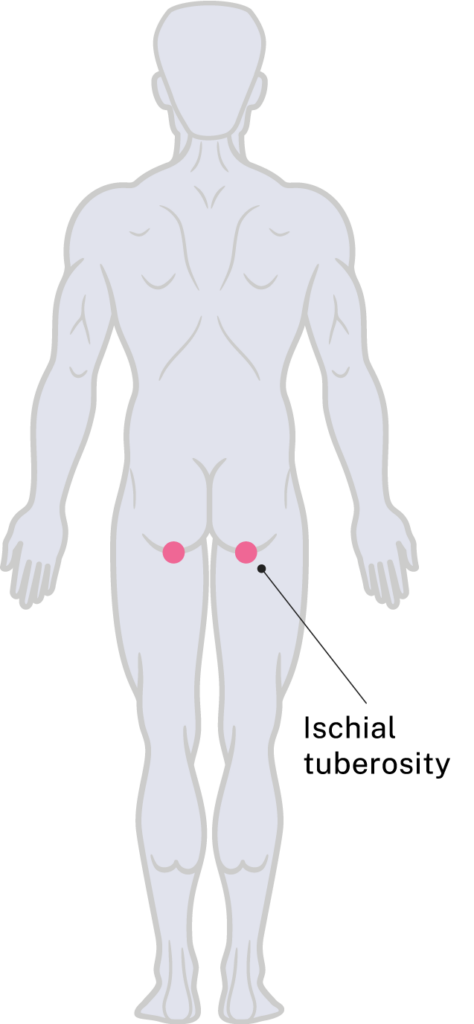
Ischial tuberosity
Specific risks
Ischial tuberosity pressure injuries most commonly occur during sitting. The ischial tuberosities bear the majority of seated body weight in a neutral sitting posture on a flat, firm surface, as they are the lowest point of pelvic contact.
Surfaces and activities that can increase pressure, shear, and friction over the ischial tuberosities include:
- Cushions, particularly if inadequate, worn, or inappropriate for the user’s needs
- Other seating surfaces such as sports chairs, car seats, hard floors, dining chairs, lounge chairs, outdoor furniture, tub transfer benches, and static shower chairs
- Transfers, especially if not well controlled or involve sliding
- Postural issues, including pelvic obliquity or scoliosis
- Infrequent or ineffective pressure relief
- Tight clothing, incontinence pads, or underwear seams
- Muscle wasting or unintentional weight loss, which reduces soft tissue protection
- Mattresses, particularly if prolonged time is spent in bed without repositioning
- Moisture and microclimate changes from heat, humidity, incontinence, or occlusive clothing, which can lead to rashes or skin breakdown that worsens with sitting
- Asymmetrical pelvic loading, such as frequent use of the dominant hand (e.g. for computer work or power wheelchair use), which may cause the pelvis to drop more on one side
These areas should be assessed by palpating for ‘boggy’, soft, or tender tissue, which may indicate early tissue damage.
Management of breakdown
- Review and identify contributing factors, including mattress and cushion quality, showering aids, other seated surfaces, transfers, clothing, muscle bulk, care routines, and continence management.
- Sitting on a commode may be appropriate following clinical review. This can be beneficial by:
- Providing stretch to the healing area.
- Supporting continuation of the bowel routine to prevent incontinence.
- Facilitating hygiene for the wound and surrounding skin.
- A postural assessment is required to identify any pelvic obliquity or scoliosis. An interim assessment can be completed during bed rest if sitting is not yet possible.
- Optimal lying positions for pressure relief include:
- Flat in supine with knees flexed up
- Prone lying, or
- Side-lying (offloading the affected area).
- Sitting in a wheelchair may be possible with custom seating. Rehabilitation Engineering Centre, Surgical Treatment and Rehabilitation Service (STARS) can be consulted for advice.
The contact details are:
email: STARS_REHABENG@health.qld.gov.au or
phone: (07) 3647 6070
Stage 3 or 4 pressure injuries may require a surgical consult.
For urgent consultation
On-call Consultant Spinal Injuries Unit,
Princess Alexandra Hospital Ipswich Road,
Woolloongabba, Queensland.
Switch: (07) 3176 2111
Ask for the SIU Registrar on business days or an on-call SIU Consultant during after-hours for the Spinal Injuries Unit.
For a review at the Spinal Injuries Unit outpatient department
Referrals can be faxed through the central intake hub on 1300 364 248.
To link with community services
Contact Spinal Outreach Team at 3176 9507 or spot@health.qld.gov.au
Check out other pressure injury locations and learn how to manage them.